On a cold Tuesday morning one March, Christian Lüscher hopped on his bicycle in the cavernous basement tunnels that snake beneath the building housing his laboratory and pedaled to the nearby Geneva University Hospitals.
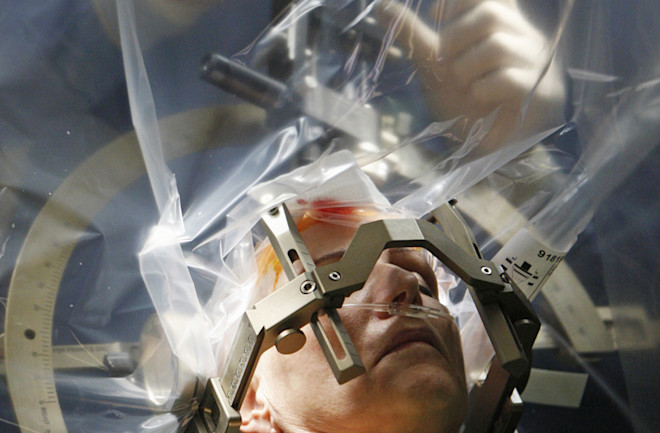
By the time he arrived in the operating room, a surgical team already had shaved a patient bald, secured a metal frame to her head and drilled two quarter-size holes on either side of her skull. She was 68, a retired U.N. employee.
Lüscher spotted her tremors immediately. From her fingers to her feet, the patient’s whole right side shook four or five times a second as neurons deep in her brain fired spontaneously, sending electrical impulses toward her motor cortex and down her spine, and causing her muscles to contract involuntarily.
Lüscher, a neurologist who has spent years treating Parkinson’s disease, was intimately familiar with her condition. Yet, as the now 52-year-old scientist watched a neurosurgeon and his team prepare to use a technique called deep brain stimulation (DBS), a very different kind of patient was never far from his mind.
For nearly 15 years, Lüscher had spent his days focused on unraveling the mysteries of drug addiction. Now he believed he was tantalizingly close to achieving something that most would have thought impossible just a few years ago. By mastering DBS, Lüscher aimed to rewire the brains of drug addicts and actually reverse their addictions.
Standing near Lüscher in the OR, a neurosurgeon consulted a monitor displaying an image of the patient’s brain. Then he slowly pushed an impossibly thin, electrode-tipped rod into her cerebral cortex, through the corpus callosum and beyond. A series of bliplike blasts began to fill the room. They were the amplified sounds of brain cells firing, picked up by the electrode and piped through a nearby speaker. Together, Lüscher and a fellow neurologist watched the Parkinson’s patient closely, and listened. When the blips began to sync with her muscle twitches, they signaled the surgeon. They were close to the neural epicenter causing the uncontrollable tremors.
The neurologist turned on a series of quick bursts of electrical current at the end of the electrode, adjusting its location and amplitude, until all the neurons in the target area began to fire. The twitching slowed. Then it stopped. He pulled out the temporary electrode and inserted a permanent one. The patient’s ordeal was almost done. She would return in three days, and doctors would insert a battery-powered device in her chest, just below the collarbone. Then they would run extension wires up under the skin of her neck to the electrodes in her brain and turn it on. The tremors and paralysis would cease for as long as the device stimulated the errant neurons corrupted by her disease.
Lüscher bid farewell to the surgical team and rode back to his laboratory, buoyed by a tantalizing vision in the back of his mind. What if treating addiction could be that simple? What would it mean to the millions of drug addicts and their loved ones? What would it mean for society?
It’s a vision that may be closer to reality than we think. In February, Lüscher reported in the journal Science that he succeeded in modifying the techniques used on Parkinson’s patients to treat cocaine addiction in mice. Lüscher gave the mice a drug that temporarily blocked a key protein in the brain. Then he applied an electrical stimulus to a neural area that in humans is just a few centimeters away from the almond-shaped spot targeted in the Parkinson’s patient, an area of the brain that scientists have come to associate with addiction. Lüscher’s results were unequivocal. The technique remodeled the mouse’s brain and appeared to have reversed the key elements of addiction.
“It’s a very pragmatic approach with a technique we hope to apply to humans in the future,” Lüscher says.
An Uphill Battle
For years, people told Lüscher that his efforts sounded quixotic, even impossible. In the 1990s, when he was a newly minted Ph.D. just entering the field, many doctors and scientists refused to acknowledge addiction was a disease.
They’d stand up in the audience after his lectures on the biochemical basis of drug addiction: physicians, social workers, psychiatrists, many of whom spent every day on the front lines of the fight against the ravages of crack cocaine, heroin and oxycodone. They’d shake their heads sadly, as if about to deliver a hard truth to a family at the clinic.
“Let’s not medicalize addiction,” they’d tell him. “You’re studying something that isn’t real. It’s psychological. There are no organic correlates.”
For generations, medical evidence proving that addiction was an actual physical brain disease had eluded scientists. Alzheimer’s causes massive brain-cell death and shrinks the outer areas of the organ. Cancerous tumors stand out against the brain’s Jell-O-like ridges, like craters on the moon. No such clues were visible in the brains of dead addicts — though they often left behind plenty of visible wreckage in their own lives. “The gold standard to determine whether someone has a disease is to do an autopsy,” Lüscher says. “But with the standard tools that pathologists have, there is not much wrong in the brain of an addict.”
Lüscher knew better than most that it was a fallacy to suggest drug and alcohol dependency was largely mental, and thus a matter of will. As a postdoc in 1996, Lüscher traveled to the University of California, San Francisco, and participated in an experiment that helped unravel the mysterious biochemical changes connected to learning and memory.
Some forms of associative learning, Lüscher and his colleagues demonstrated, were reflected in the appearance of microscopic proteins called AMPA receptors. These receptors bloomed at the tiny cleft where two neurons meet, known as the synapse, and “wired” the neurons together with a stronger bond. Lüscher was convinced that these same processes would someday explain addiction.
So, in those early lectures, Lüscher would stand in front of the doubters, listen politely to their criticism, and then explain why they were wrong. Addiction didn’t kill neurons; it somehow remodeled the connections between them in a devastating and maladaptive way. And someday soon, scientists would find a way to prove it.
That day finally arrived in 2001, when a UCSF team electrified the field of addiction research by isolating distinct, long-lasting biochemical changes that appeared in the brains of mice after exposure to cocaine. This “addiction trace” was proof that addiction was a medical condition; the evidence of the mysterious mechanisms in play had been slowly building for years. The Brain’s Sweet Spot
The discovery that sparked the age of modern addiction research occurred entirely by accident. At a McGill University lab in the early 1950s, postdoc James Olds was hunched over a rat, trying to attach electrodes to the area of its brain he suspected was associated with pain.
Olds and graduate student Peter Milner planned to zap the rat every time it wandered into a specific corner of the cage. But far from recoiling when the electrode was activated, the rat seemed to enjoy the experience. Instead of avoiding the corner, the rat hurried back to it. When the two men investigated further, it turned out that during setup, the electrode had jarred loose and lodged into another nearby area of the brain.
Olds and Milner modified the experiment, offering the rat a way to self-administer the pulse by pressing a lever. When they placed the electrode at a particular sweet spot, some rats pressed the lever hundreds of times an hour. In subsequent experiments conducted by Olds, some rats pressed the lever as many as thousands of times an hour. They ignored food and water. Some self-stimulated until they collapsed from exhaustion.
Olds hypothesized that the area consisted of interconnected circuits of brain cells that could be excited by the satisfaction of basic drives, circuits of the brain that perhaps contained the very seat of hedonism itself. A newspaper gave the area its famous name: the “pleasure center.”
It wasn’t much of a stretch to relate the behavior of these compulsively self-stimulating rats to that of human alcoholics or drug addicts on a binge.
In the 1970s, researchers began to home in on a specific neurochemical substance at work in the brain. Scientists already knew the brain’s main signaling agents were neurotransmitters, chemical messengers released by a neuron when it’s activated. These messengers travel across the synapses connecting the excited neuron to its neighbors and bind with proteins on the surfaces of the neighboring cells. This, in turn, affects how many positively charged ions are allowed into these neighboring cells’ interiors, and how likely they are to fire electrical pulses of their own. When they do, they release neurotransmitters to their neighbors, which causes them to switch on, and so on.
Researchers thought these neurotransmitters were involved in the compulsive behavior of the drug-seeking mice. Roy Wise wanted to figure out which one. Whereas Olds stimulated rats’ brains directly with electrodes, Wise, then a researcher at Concordia University in Montreal, did so indirectly with intravenous tubing used to deliver drugs like amphetamine. He hit the jackpot when he fed rats pimozide, a drug that blocks the neurotransmitter dopamine. On low doses, the rats tried pressing the lever faster to increase the dose of amphetamines. When Wise fed them large doses of pimozide, they lost interest. The implication seemed clear: Dopamine was needed for amphetamines to stimulate the pleasure center, and its presence somehow helped spur the compulsive behavior.
Researchers also demonstrated that if you produced lesions in the brain’s supply center of dopamine, the rats lost interest in amphetamines. The ventral tegmental area (VTA) and a related adjacent area called the nucleus accumbens (NAc) were crucial to the dopamine system. The effort to definitively prove and flesh out the theory — known as the dopamine hypothesis — became the linchpin of addiction research for the next 30 years.
By the mid-1990s, most addiction researchers came to believe that dopamine’s role is more complex than a simple pleasure juice. Dopamine serves as a learning signal that helps animals remember pleasurable experiences and develops the motivation to repeat them. But this signal somehow goes awry with addiction. Research also has demonstrated that dopamine needed to be present for rats to remember unpleasant experiences, such as electric shocks. When an animal experiences any intense stimulus that is worth remembering, dopamine is released in the brain.
“One of the things that has been stressed in recent literature is that the dopamine system is activated by stress,” says Wise, who is now at the National Institute of Drug Abuse (NIDA). “These [stressors] are not pleasant, and yet they stamp in memory as effectively as pleasurable experiences. Dopamine is responsible in both cases.”
Memory and Relapse
One of the most vexing aspects of addiction is relapse. It’s not just that addiction overcomes resolve, even when a relapse threatens livelihoods, relationships and the addict’s very life. It’s that the compulsion to use lingers long after the drug of choice has left the addict’s body. How do the demons of this invisible disease persist when no physical trace can be found?
To many, the answer isn’t complicated: It’s as simple as bad character, selfishness. But in recent years, addiction researchers have compiled mounting evidence showing that addiction is a maladaptive form of learning somehow etched permanently into the most primitive areas of the brain. The chemical tool that leaves that mark, researchers long suspected, is dopamine. Yet to prove it, they needed to find evidence of the mark itself.
To do that, first they would need to answer a more basic question: If addiction is a maladaptive form of learning and memory, how precisely do normal learning and memory work?
It was a question at the heart of research in the labs of two UCSF researchers, Rob Malenka and Roger Nicoll. Their work, in many ways, would set the stage for the revolution now overtaking the field of addiction research. Malenka and Nicoll knew that our memories connect to one another through a vast matrix of associations, a principle poetically articulated by neuroscientist Carla Shatz: “Cells that fire together, wire together,” she wrote. “Cells that fire out of sync, lose their link.” Put another way, the coincidental firing of two neurons close to each other somehow causes the connections between them to strengthen. That strengthening at the synapses makes them more likely to fire together in the future.
In the 1990s, Malenka and Nicoll were at the center of the race to unravel the precise chemical processes underlying this phenomenon, known as long-term potentiation (LTP). The key to solving the mystery lay in understanding how signals are passed between neurons. A neuron fires only when the ratio of positively to negatively charged ions inside its membrane rises above a certain point. For that to happen, millions of tiny, electrically charged ions must get inside the cell through specialized gated proteins.
In the hippocampus and the amygdala, areas of the brain thought to be associated with episodic memory, researchers had shown that the chemical signaling agent called glutamate acts like a key in the lock of some of these protein “flood gates.” Malenka and Nicoll focused on AMPA and NMDA, two different kinds of protein receptors on the surface of neurons that can bind with the neurotransmitter glutamate.
AMPA receptors will bind with glutamate any time it is released by a neighboring cell. The gates of AMPA receptors will open, and positively charged ions flood into the cell. But under normal circumstances, an NMDA receptor is like a locked door with a second door behind it. Even though glutamate can bind to NMDA receptors, it cannot open NMDA receptors’ gates on its own because the gates are usually blocked by magnesium ions. But there is an exception. If a neuron is already firing, its NMDA receptors undergo temporary changes. During spikes, the magnesium ions will detach at all synapses. The opening of this inner second door allows access to the interior of the cell.
The gates of the NMDA receptors are structured differently from those of AMPA receptors. And when NMDA gates open, calcium ions that cannot fit through AMPA receptors’ openings suddenly flood the neuron’s interior. The presence of calcium inside the cell, Malenka and Nicoll believed, acts like a cellular starting gun, setting off a complex cascade of chemical processes that results in LTP.
Malenka and Nicoll, along with their team, demonstrated that LTP occurs when calcium enters the cell and new AMPA receptors move to the cell surface. The presence of these additional receptors makes the cell more sensitive to future releases of glutamate from its neighbor.
What’s more, by controlling the timing of an electrical stimulus, Malenka and UCSF researchers conclusively demonstrated that they could cause more AMPA receptors to appear on the outer membrane of a receiving neuron — or, conversely, to disappear.
Malenka then began to wonder if similar mechanisms might be at work with addiction, and he began a series of experiments that finally led to the smoking gun.
In 2001, UCSF researchers injected mice with cocaine, unleashing a flood of dopamine. Then they prepared mouse brain slices from a group of neurons in the dopamine production center, at 24 hours and every day thereafter. As they scrutinized the magnified slices of brain taken from their coked-up mice, Malenka and his colleagues collected the minute electrical recordings that documented the response of one neuron to the firing of its neighbor.
What they found exhilarated the nascent field of addiction research. The initial activity boost caused the neurons producing the dopamine to become twice as sensitive to additional stimulation from neighboring neurons for days, long after the cocaine had left the body. Only at 10 days did all trace of the changes dissipate. Next, the researchers administered a drug that blocked NMDA receptors from responding to signals from neighboring cells when they introduced the cocaine, and no such sensitization occurred.
This was the first evidence that just one recreational dose of cocaine could hijack the mechanism that lay at the very basis of memory and learning — the strengthening of the connections between cells.
“This was the first step — it was the tip of the iceberg,” recalls Malenka, now at the Stanford School of Medicine. “Addiction is a maladaptive form of memory and learning.” Clue to a Cure
Studies demonstrated that the changes in the brain’s dopamine production area, or VTA — though crucial to the development of addiction — also triggered a cascade of biological processes that resulted in permanent changes in the nucleus accumbens (NAc), the area downstream that is closely linked to motivation and goal-directed behavior. These changes, in this crucial area of the brain, might help explain why addicts lose interest in natural rewards, some researchers suggest. (Addiction also causes changes in other areas of the brain, such as the cortex and the limbic system, that further influence these behaviors.)
In 2008, Marina Wolf, a leading addiction researcher who chairs the neuroscience department at the Chicago Medical School at Rosalind Franklin University of Medicine and Science, examined the key mystery of the field: the phenomenon of recurrent relapse, which strikes even those who have every intention of quitting their drug of choice. Wolf and her team trained rats to poke their noses in a hole to receive an intravenous dose of cocaine, which triggered a light cue. After 10 days of teaching each rat to associate the light with receiving cocaine, the team removed the cocaine tube, waited a day, and began measuring how hard the rat was willing to work to get the cocaine when the lights went on. The more times the rat poked the hole, the more motivated the rat was to get the cocaine and thus, the stronger its urge.
To those outside the field of addiction research, the timing of this motivation might seem counterintuitive. But researchers at NIDA demonstrated that there seemed to be an incubation period: The craving waned, but a dramatic spike in cravings followed. “In rats that have taken a lot of cocaine, craving becomes stronger rather than weaker as the withdrawal period gets longer,” Wolf says. Similar research has shown that “if you go out a month and show rats the cue, the craving is much more. And it peaks at three months. Even six months down the line, the craving is stronger than at one day.”
Indeed, by examining brain tissue and slices from the cocaine-addicted rats at various stages of withdrawal and craving, Wolf and her colleagues discovered that the incubation period and the subsequent spike in craving appeared to correlate with the appearance of atypical AMPA receptors on the surface of neurons in the NAc, which could help explain cocaine craving. These atypical AMPA receptors were missing a key subunit, called GluA2, that caused a change in shape and allowed calcium ions to enter the cell. As a result, when the animals see the cue and glutamate is released, the NAc neurons responded far more strongly to the cue, and the rats exhibited a far stronger craving. But the change also had other implications. Since calcium ions usually enter a cell through NMDA receptors only when a cell is already firing, the atypical AMPA receptors, by allowing calcium to enter the cell, disrupted the entire biochemical process of learning and memory in the primitive areas of the brain that are part of the very seat of motivation itself.
“Changing the way learning occurs in the nucleus accumbens is a pretty serious thing for the [future behavior] of the organism,” Wolf says.
This period for sensitivity to relapse was counterintuitive, yet familiar to anyone who has watched a friend triumphantly quit cigarettes, alcohol or an addictive drug for a couple of weeks, only to relapse inexplicably just when it seemed they had beaten the bug.
“When we blocked these unusual AMPA receptors with a drug before testing the rats, we reduced their craving almost to normal levels,” Wolf says.
Switch on the Lasers
Wolf’s 2008 paper got Lüscher thinking. Might it be possible to somehow reverse the changes by artificially stimulating the NAc in a way that mimicked the way memories fade in the brain?
Lüscher proposed this seemingly farfetched idea to his 15-member lab team. He had just returned from a half-year sabbatical at Stanford University, where he mastered optogenetics. The technique genetically infuses individual brain cells with light-sensitive proteins (called rhodopsin) that would open up and cause the cells to fire — or cease doing so — in response to specific colors of focused light delivered through fibers.
By 2011, grad student Vincent Pascoli began his first experiments. Inspired by the idea that “neurons that fire apart, wire apart,” Lüscher instructed Pascoli to attempt to artificially induce the chemical reactions known to weaken connections between two neurons. They aimed to prove that stimulating one synapse with an electrical pulse once a second for 10 minutes would weaken connections.
Previous experiments linked cocaine addiction with more drug seeking and increased sensitivity to the drug. One way to measure increased sensitivity was to inject a mouse with cocaine, place the mouse on a circular track, and count how many times it runs around the track. More sensitive mice are likely to run around the track twice as fast as a mouse receiving its first cocaine injection.
In preparation for his optogenetic experiment, Lüscher placed the mice on the track, timed their runs, fed them cocaine and put them back on the track. He then took slices of each mouse’s brain and measured whether it led to an increase in the amount of electricity passing between neurons in the accumbens and the prefrontal cortex. The increase in electricity — and thus the presumed sensitivity of the mouse to cocaine — lined up perfectly with the rate at which the mice ran around the track.
When Lüscher and his team repeated the experiment, they followed up the cocaine with optogenetics. They drilled tiny holes in the mouse skulls and inserted light fibers through the brain tissue until they reached the NAc, where the neurons had been genetically modified to contain light-sensitive, gated proteins. Then Lüscher and his team shined a blue light through light fibers, selectively stimulating some of the neurons. The stimulated neurons fired, releasing glutamate. But the low frequency of the firing and the amount of glutamate released wasn’t enough to cause the neighboring neurons to fire.
In other words, Lüscher’s protocol created the conditions that caused the neurons to fire apart, which made them wire apart. Doing so, he hoped, would result in a disappearance of AMPA receptors from the surface, weakening the connections.
The results were clear. When they placed the mice back in the maze and gave them cocaine, they responded as if it was a first-time injection. The addiction sensitization had disappeared.
Lüscher’s work, published in 2011 in Nature, implied for the first time that optogenetics could be used to reverse LTP, allowing researchers to manually erase learned behaviors. In a 2014 paper, Lüscher’s team demonstrated that mice taught to self-administer cocaine over a longer time period also responded. Not only did this protocol lead to the removal of the defective AMPA receptors, but when AMPA receptors returned, they were normal again.
Although there were still likely plenty of abnormalities present in his treated mice, Lüscher’s 2011 optogenetics paper was among the first indicating we may be approaching a cure, or at least an age of powerful new interventions for addiction. In 2014, Wolf and her colleagues published work in rats suggesting that relapse in cocaine addicts also could be prevented by administering a non-toxic experimental compound that leads to the removal of the calcium-permeable AMPA receptors for about a day, thus reducing the ability of cocaine-related cues to trigger powerful craving that can lead to relapse.
“These compounds would not cure addiction. They would be something a recovering addict could take to maintain abstinence prior to entering a situation full of cues that might trigger relapse,” Wolf says. “But right now, there are just no treatments for cocaine addicts, so even just a day of protection would be of great help.”
Since optogenetics is considered far too invasive for humans, Wolf’s technique had a clear advantage over Lüscher’s. But Wolf’s approach also had a downside: The injected drug traveled all over the brain, unlike Lüscher’s localized optogenetic approach, which Lüscher believes also could lead to long-lasting changes.
Lüscher knows it will likely be many years before optogenetics is modified so it could be used in humans. Instead, he is focused on mastering DBS, which uses electrodes to stimulate groups of neurons rather than individual brain cells. Although some researchers have attempted to use DBS on addicts in various parts of the brain and say they have promising anecdotal results, no large-scale studies have been conducted, Lüscher says. And none of these experimenters has done so with the intent of reversing the synaptic changes brought on by the use of cocaine or other drugs of addiction.
Researchers still aren’t sure precisely why DBS works in Parkinson’s patients. The strong burst of electrical activity somehow immobilizes the neurons that cause tremors. And this is the same protocol that others have tried to apply to different parts of the brain to treat addiction.
Lüscher’s approach is fundamentally different. He radically slows down the pace of the electrical stimulation of brain cells to match the rhythm of activations that he used to reverse addiction with optogenetics. Rather than tiring out neurons to temporarily immobilize them, as is done with Parkinson’s, Lüscher is using DBS to remodel the connections between neurons because “cells that fire out of sync, lose their link.”
DBS is far less precise than optogenetics, and the electrical field its electrodes create is larger and stimulates many more neurons than necessary. But Lüscher has discovered that if he administers a drug that temporarily blocks neurons from binding with dopamine, and then administers DBS, he is able to replicate his findings with optogenetics in mice.
“The two together still are not exactly the same as optogenetics, but it does the job,” Lüscher says of DBS and the drug. “So it’s a very pragmatic approach to try to translate and emulate what we have been successfully doing with optogenetics.”
“It’s a still long shot to go from optogenetics in mice to doing this on humans,” Lüscher said as he sat in his lab one morning. “I am not sure if that will happen in my lifetime [as a scientist]. But DBS is an intermediate step. I am optimistic.”