Every embryo begins as a single fertilized egg, which develops into a human body consisting of trillions of cells, each one specialized to carry out specific functions. Since embryonic stem cells can differentiate into any type of tissue, they have the potential to treat an almost unending array of medical conditions — replacing damaged or lost body parts or tissues, slowing degenerative diseases, even growing new organs. Researchers working to understand how to manipulate this powerful tool get their supply from stem cell lines, groups of stem cells derived from animal or human tissue that can reproduce themselves indefinitely.
What Are They?
Stem cells can morph into all manner of specialized tissue cells. They are prized for their potential to treat many different kinds of medical conditions, as well as serving as a testing ground for drugs.
Three Distinct Types:
Embryonic stem cells: They can turn into any of the body’s 220 different cell types, meaning they are pluripotent.
Adult stem cells: They have less flexibility and “stemness” to change into different cell types, but they can still produce new cells, specialized to become part of a particular organ or tissue, such as muscle cells or neural cells.
Induced pluripotent stem cells: These genetically reprogrammed skin cells regain the “stemness” of embryonic stem cells.
The Debate
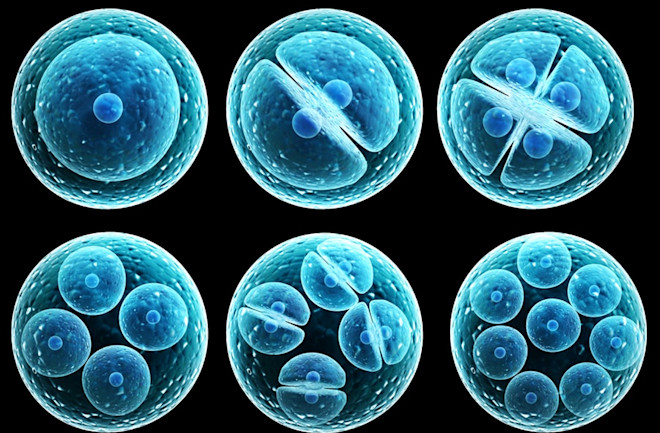
In 1998, scientists figured out how to derive human embryonic stem cells (ESCs) for medical research, and the method kicked off an intense debate. To access ESCs, researchers puncture the outer walls of early stage embryos, known as blastocysts, and reach into the inner cell mass to extract them — a process that destroys the rest of the embryo. The stem cells are then cultured and induced to develop into any one of the body’s cell types. Opponents who believe that human life begins the moment a sperm fertilizes a single egg decry the destruction of early stage embryos.
Proponents of ESC research counter that most of the new cell lines could be derived from donated, unused human embryos created by couples seeking fertility treatment, and that more than a third of zygotes fail to implant after conception, so those would be lost by chance anyway.
In 2001, President George W. Bush limited the use of federal funds for research done with new ESCs. The debate has quieted down since then. In 2007, scientists demonstrated it was possible to reprogram adult skin cells to behave like embryonic ones. Induced pluripotent (iPS) cells are not exactly the same as ESCs, but evidence has continued to mount that they are nearly functionally equivalent, leading many scientists to make the switch.
A Short History
1961 Ernest McCulloch and James Till isolate stem cells from the bone marrow of mice.
1962 John Gurdon removes the nucleus from the egg cell of a frog and replaces it with a nucleus of a mature cell from a tadpole. It still grows into a new frog, proving that mature cells still contain the genetic information needed to form new cells.
1981 Martin Evans and Matthew Kaufman isolate mouse embryo stem cells and cultivate them in the laboratory. Gail Martin also demonstrates this around the same time and coins the term embryonic stem cells.
1998 James Thomson isolates stem cells from human human embryos.
2006 Shinya Yamanaka identifies and activates a small number of mouse genes in the cells of connective tissue, showing they can be reprogrammed to behave like immature stem cells.
2007 Yamanaka and Thomson succeed in reprogramming adult human skin cells into induced pluripotent stem cells.
2012 Gurdon and Yamanaka share the Nobel Prize in Physiology or Medicine.
Today’s Hot Areas
Stem cells can be manipulated to serve many objectives, but they need the right conditions.
“Stem cells take their cues from the nutrients they receive, the intensity of electrical impulses they feel, how much oxygen they get and even how much movement they experience,” says Gordana Vunjak-Novakovic of Columbia University. “All these factors, in addition to the physical dimensions of their surroundings, indicate to the stem cells what part of the body they’re in. We need to create an artificial environment that mimics all of that.”
As scientists decode and find ways to replicate these environments, they are pioneering a number of new treatments that can transform medicine, showing how they can be used to regenerate damaged tissue, create new muscle where there was none before — even grow “organelles” that can be used to test new drugs.
Retinal Epithelial Cells
Age-related macular degeneration is the leading cause of blindness for people over 65 in the United States and affects more than 15 million people. The disease occurs when a layer of cells at the back of the eye, called the retinal pigment epithelium, degenerates.
One researcher has found a way to cultivate retinal stem cells and developed an implantation technique that aims to reverse the disease’s progression, by injecting about 50,000 healthy cells behind the retinas of mice with damaged retinas.
“By putting in healthy cells, we can basically stop and prevent the degeneration of the photoreceptors,” says Sally Temple, the co-founder and scientific director of the Neural Stem Cell Institute in Rensselaer, N.Y.
Three years after publishing a groundbreaking paper in which she isolated adult retinal pigment epithelial stem cells, Temple is in preclinical trials with rats. She hopes to launch human trials in the next two years.
Stem cell source: Temple obtains her raw materials from eye banks. Many individuals donate eyes for corneal transplants; often, corneas are removed from the front of the eye, and the back part, with the retina, is tossed. From these normally discarded materials, Temple extracts adult stem cells and cultivates them in thin sheets. (Masayo Takahashi in Japan has launched a parallel effort that uses iPS cells.)
Muscle
Muscle is one of the most regenerative organs in the body, and it is bustling with adult stem cells standing ready to repair the many rips and disruptions that occur from exercise. Researchers have long struggled with a mystery, however. When they cultivate muscle stem cells in a dish, the cells often lose their ability to differentiate into muscle cells. Depending on the growth conditions, the artificially produced muscle loses its innate capacity to repair itself.
Duke University’s Nenad Bursac believes he may have found the solution. The key is to create a niche, 3-D microenvironment that encourages some cells to become muscle fibers and others to go into what he calls a “quiescent state.”
“They don’t do much, but if there’s an injury, they jump in, they proliferate, and they rebuild the muscle,” says Bursac, a professor of bioengineering. He hopes that one day his technique can be used to help treat patients with muscular dystrophy, in which their bodies attack their own muscle.
Stem cell source: Bursac obtains muscle through a biopsy, soaks the cells in a cocktail of factors and then adds some to a 3-D environment, a hydrogel that mimics the geometrical shape of a blood clot. This primes the cells to fuse, causing some to quickly become muscle fibers and others to stick to those fibers and remain stem cells in their quiescent states.
“Through this kind of a combination of things,” Bursac explains, “we managed to get tissue-engineered muscle but with a capacity to have a stem cell function and be able to regenerate the muscle after injury.”
Neurons
In the pharmaceutical industry, new stem cell technologies are allowing scientists to examine brain disease in the petri dish while also testing the effectiveness and safety of potential drugs in new ways.
“You just don’t have access to the brain cells of 500 children with autism,” says Ricardo Dolmetsch, the global head of neuroscience at the Novartis Institutes for BioMedical Research. “The next best thing is to make them.”
Dolmetsch is using iPS cells to study psychiatric and neurodegenerative diseases, and to screen for drugs that might work to treat them. He and his colleagues take skin cells or blood cells from those with the conditions they wish to study. They turn those cells into stem cells and coax them to become neurons. Because every cell from an individual carries the same genetic blueprint, these neurons should be identical to the neurons in each patient’s brain — and should carry the same defects that spur disease. They can then be used to test drug interventions or to test hypotheses about the causes of disease.
“Now that we have the capacity to make cells for many, many people in an automated way, we can effectively do a kind of clinical trial on their cells before we actually expose the patient to the drug,” Dolmetsch says. “Ultimately, it should allow us to produce less expensive drugs, more quickly.”
Stem cell source: Obtained from skin or blood cells of patients. These samples are then infected with modified viral vectors, essentially re-engineered to contain pieces of DNA that activate specific genes and cause the samples to behave like embryonic stem cells. Dolmetsch exposes these stem cells to a variety of different growth factors that mimic those that induce stem cells to become neurons during normal development.
Lung Cells
The architecture of a lung is as complex a structure as a Minotaur’s maze. We inhale air through the trachea, a single passage, which quickly branches into smaller offshoots that project branches of their own. There are 23 generations of branching in the human lung, and hundreds of millions of air sacs 200 microns in diameter, each one filled with capillaries that absorb oxygen into the blood.
So when building new lungs, Yale bioengineer Laura Niklason prefers not to start from scratch. After taking lungs from a donated cadaver, she soaks them in a combination of detergents and strong salt solutions to wash away the cellular components. What’s left behind is a raw scaffold composed of structural proteins. Once the scaffold has been cleansed, she suffuses it with stem cells and places it in a bioreactor. It reproduces the lung’s natural environment in the body, from the physical forces to the chemical soup — all to help manipulate stem cells to mature into specific tissue.
“Blood perfuses through our lungs,” she explains. “So we had a setup so that we could perfuse the lung tissues and allow them to breathe as well, because breathing is important for lung development. Then we spent a lot of time working on the soup.”
Once the stem cells are created, Niklason relies on different chemical markers left behind in the decellularized lungs to guide the stem cells to their correct locations.
“If you decellularize the lung carefully, you actually leave behind footprints from the cells,” she explains. “It’s probably partly geometry. A lot of it is the local proteins, the local matrix proteins, that are sitting there left over after you take the cells away.”
Stem cell source: With rats, Niklason has relied on lung cells from other animals to repopulate the scaffold. But with humans, she is using iPS cells and has been working to develop the correct protocols to induce her stem cells to differentiate into different kinds of lung tissue.